Coxarthrosis is a common degenerative-dystrophic disease of the hip joint, in which, due to age-related changes or other factors, there is a gradual destruction of the articular joint of the femoral head and the pelvic acetabulum . It is accompanied by pain and limitation of the amplitude of movements of variable severity, which depends on the stage of development. And if at the initial stages it is possible to cope with coxarthrosis with conservative methods, then at the third stage it is possible to save the situation and maintain the working capacity of the hip joint, that is, avoid disability, only by performing an operation. .
It belongs to the number of arthrosis and can be accompanied by the development of similar processes in other joints, and this pathology accounts for about 12% of all diseases of the musculoskeletal system. But the term "coxarthrosis" can only be used to describe degenerative dystrophic changes in the hip joint.
what is coxarthrosis
Coxarthrosis is a complex pathology of one or both hip joints, in which the cartilaginous layers that cover the femoral head and the acetabulum are destroyed, leading to a decrease in the size of the joint space. As the disease progresses, the appearance of deformations of the bone surfaces and the formation of bony growths on them, called osteophytes, are observed.
Coxarthrosis is the second most common disease of the musculoskeletal system. More often, only gonarthrosis is diagnosed, that is, a degenerative dystrophic change in the knee joint. However, the probability of disability in coxarthrosis is significantly higher.
The entire hip joint is enclosed in a specific box, which is called the joint capsule. It has a so-called synovial membrane, which produces synovial fluid. This fluid is essential for the proper functioning of the joint, since it not only lubricates the hyaline cartilage, but is also a source of nutrients for it.
Normally, cartilage is constantly worn down and immediately restored due to the continuous regeneration process, which is carried out with the help of substances that enter from the synovial fluid. But with injuries or age-related changes, the rate of regeneration processes slows down, which leads to gradual wear of hyaline cartilage and the development of coxarthrosis.
This is due to changes in the amount of synovial fluid produced and its composition. Under the influence of adverse factors, it becomes thicker and is produced in a smaller volume. As a result, the synovial fluid is no longer able to provide the hyaline cartilage with all the substances it needs in the right amount, leading to its rapid dehydration and thinning. Gradually, the strength and elasticity of the cartilage decrease, the areas of delamination of the fibers that form it, cracks form in it, and the thickness also decreases. These changes can be noted during instrumental diagnostic methods, in particular, the narrowing of the joint space is striking.
Joint space narrowing causes increased friction between the bony structures that make up the hip joint and increased pressure on the already degrading hyaline cartilage. This causes even more damage, which affects the function of the joint and the person's condition, since the deformed areas prevent the femoral head from sliding easily into the acetabulum. As a result, there are symptoms of coxarthrosis.
If left untreated, the pathological changes worsen and the hyaline cartilage wears down more and more. Subsequently, in some areas, it completely disappears, which leads to the exposure of the bones and a sharp increase in the load on the joint. Since when moving inside the acetabulum, the femoral head rubs directly against the bone, this causes the appearance of intense pain and a strong limitation of mobility. In this case, the pressure of bone structures on each other leads to the formation of bone growths on their surface.
The formed osteophytes can have sharp parts that can injure the muscles and ligaments surrounding the hip joint. This gives rise to the appearance of severe pain both directly in the joint area and in the groin, buttocks and thighs. As a result, the patient respects the injured leg, puts less pressure on it and tries to avoid making unnecessary movements with it. This causes the development of muscle atrophy, further exacerbating mobility disorders and ultimately leading to lameness.
Causes

There are many reasons for the development of coxarthrosis, although in rare cases it occurs against the background of the absence of prerequisites. In this case they speak of the presence of primary or idiopathic coxarthrosis. In the vast majority of cases, secondary coxarthrosis is diagnosed, which becomes a logical consequence of a number of diseases or changes in the state of the musculoskeletal system. It can be caused by:
- hip joint injuries of various nature, including fractures, dislocations, contusions, sprains or torn ligaments;
- hard physical work, professional sports, especially weightlifting, skydiving, jumping sports;
- sedentary lifestyle;
- being overweight, which significantly increases the load on the hip joints;
- foci of chronic infection in the body;
- congenital malformations of the hip joints, such as dysplasia or dislocation;
- metabolic pathologies and endocrine disorders, in particular gout, diabetes mellitus, especially in decompensated form;
- aseptic necrosis of the femoral head, which can be the result of a fracture of the femoral neck, especially during conservative treatment;
- inflammatory joint diseases, including rheumatoid arthritis, bursitis, tendinitis;
- spinal diseases;
- genetic predisposition;
- the presence of bad habits, especially smoking.
However, the main cause of coxarthrosis remains the inevitable age-related changes, and the presence of the above factors only increases the probability and speed of its development.
Symptoms of coxarthrosis

The disease is characterized by a gradual progression with a systematic increase in the intensity of symptoms. Therefore, in the initial stages, it can be asymptomatic or only occasionally cause anxiety to patients, but later the condition of the hip joint worsens, which leads to an increase in the severity of signs of coxarthrosis up to excruciating pain. and significant limitation of mobility. .
So, degenerative-dystrophic changes in the hip joint are accompanied by:
- Pain of varying strength, arising initially after physical exertion or walking and disappearing after rest. Gradually, the severity of the pain syndrome increases, it appears more often, lasts longer, and the periods between the moment of applying the load on the joint and the onset of pain are reduced. Later, the pain is present almost constantly, even at rest, and becomes unbearable. Increased pain is characteristic at any stage of the development of the disease during hypothermia and heavy lifting.
- Restrictions in the mobility of the hip joint, which are initially manifested by minor difficulties in the implementation of rotational movements of the leg. Over time, morning stiffness appears, which disappears after the patient "disperses". This may be accompanied by the appearance of edema in the hip joint. As the disease progresses, the mobility restrictions become more pronounced and persistent, that is, they do not disappear after a rewarming. Patients note a decrease in the amplitude of leg movements, and subsequently completely lose the ability to perform certain movements.
- Crunch in the hip joint, which appears when walking or doing physical work, especially when doing extension. It becomes the result of friction of bare bone structures with each other, which is accompanied by a sharp increase in pain.
- Spasm of the thigh muscles, leading to diffuse pain in the thigh. This may be the result of various intra-articular disorders coming together, including nerve compression, overstretching of the ligaments surrounding the joint, as well as the development of synovitis, i. e. inflammation of the synovial membrane and accumulation of inflammatory tissue. effusion into the cavity of the hip joint.
- Lameness, which is initially the result of the patient's unconscious desire to reduce the load on the diseased joint and transfer weight to the healthy leg in order to prevent the onset or intensification of pain, and then the development of muscle contracture. The latter phenomenon occurs already in the late stages of coxarthrosis and leads to the fact that the patient cannot fully straighten the leg, and, moreover, keep it in this position. Therefore, the lower limb with the affected hip joint is constantly in a slightly bent position, which leads to lameness.
- A decrease in leg length, which already occurs mainly with severe degenerative dystrophic changes in the hip joint, accompanied not only by a narrowing of the joint space, but also by flattening of the femoral head, muscle atrophy. As a result, the diseased leg becomes shorter than the healthy one by 1 or more centimeters.
Coxarthrosis can affect either one hip joint or both at the same time. But if in the first case the symptoms of the disease will be observed only on one side, then in the second they will be not only bilateral, but also differ in intensity. It depends on the degree of destruction of each hip joint.
Degrees of coxarthrosis
The nature of the manifestations of the disease depends on the stage of its development. In total, there are 3 degrees of coxarthrosis, of which the first is considered the easiest. In the initial stages of the appearance of degenerative-dystrophic changes in the hip joint, only episodic pain can be observed. As a rule, this occurs after intense physical exertion, playing sports or a long walk. For this reason, patients do not usually pay attention to them, attributing them to fatigue and considering them to be age-related changes. In this regard, coxarthrosis of the first degree is diagnosed only in isolated cases, which usually occurs during an examination for another reason.
As the disease progresses, its symptoms intensify and already with coxarthrosis of the second degree they make themselves felt. This stage of development of the pathology is characterized by a narrowing of the joint space by 50%, as well as the appearance of signs of deformation of the femoral head with its displacement.
With further progression of the pathology, the joint space narrows even more, and with the third degree of coxarthrosis it is almost completely absent. This is already accompanied by the formation of multiple osteophytes. At this stage of the development of the disease, the pain becomes not only strong, but unbearable, and often occurs even in a state of complete rest, even at night. Since the hip joint is severely deformed, its elements can infringe on the nerves that pass here, which causes pain radiating to the groin, buttocks, as well as the thigh and even the lower leg. This also results in the inability to move independently without the use of assistive devices such as crutches or canes.
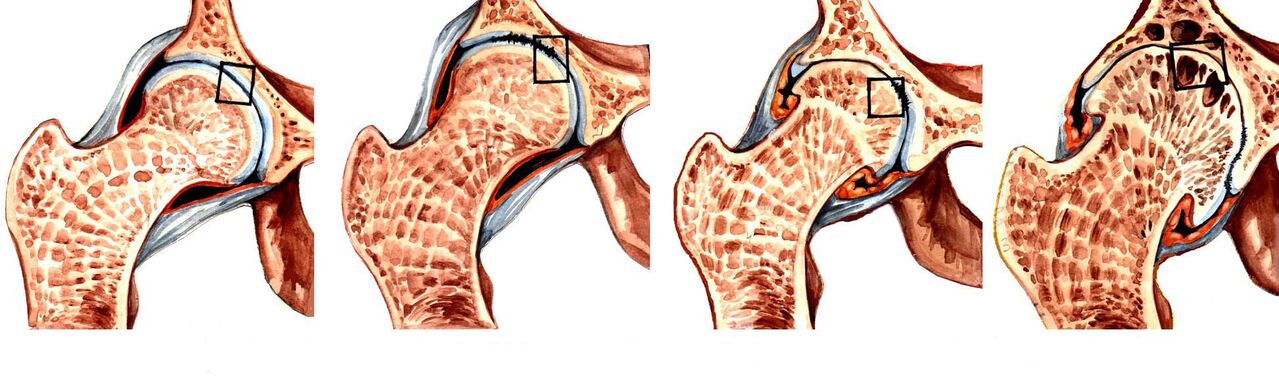
Third degree coxarthrosis is a direct indication for surgical treatment. If the operation is not performed on time, the femoral head will firmly fuse with the surface of the acetabulum with osteophytes. This will lead to a shortening of the leg, the complete absence of the possibility of independent movement, since the joint will completely lose mobility, that is, disability.
Diagnostics
If signs of coxarthrosis appear, it is recommended to contact an orthopedist as soon as possible. Initially, the doctor will interview the patient and find out the nature of the complaints, and then proceed to the examination and functional tests, comparing the length of the legs. As a general rule, the data obtained are sufficient to speak with a high degree of confidence about the presence of coxarthrosis.
But since such a clinical picture can accompany a number of other diseases of the hip joints, both inflammatory and non-inflammatory in nature, instrumental diagnostic methods are required. With its help, a specialist will be able not only to confirm the presence of coxarthrosis, to differentiate it from radicular syndrome caused by pathologies of the spine, but also to correctly assess the degree of its development, which means choosing the most effective treatment tactics. .
Today for the diagnosis of coxarthrosis are used:
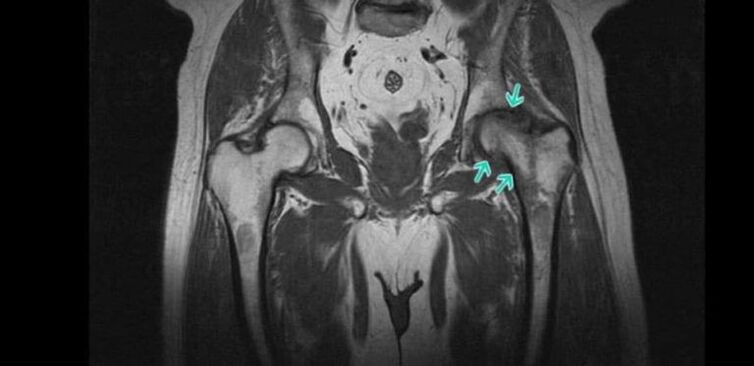
- Radiography of the hip joints - the resulting images allow you to detect signs of destructive changes, the presence of osteophytes, the nature of the deformation of bone structures, and measure the thickness of the joint space.
- CT is a more modern method of diagnosing bone pathologies and provides clearer data than radiographs, but is more expensive. Therefore, CT is prescribed in controversial cases, when it is necessary to clarify the diagnosis and the degree of destruction of the hip joint.
- Magnetic resonance imaging is a very informative method of examining the joints and provides the maximum amount of information about the state of the joint and all its structures, especially the hyaline cartilage, ligaments and the characteristics of the blood supply.
Patients are prescribed a number of laboratory tests, including KLA, OAM, rheumatic tests, biochemical blood tests, and others.
Conservative treatment of coxarthrosis

When coxarthrosis of 1 or 2 degrees is diagnosed, treatment is carried out using conservative methods. For each patient, they are selected individually, taking into account the detected comorbidities. For this reason, it may often be necessary to consult not only an orthopedist, but also doctors from other specialties who will select the necessary treatment to combat concomitant diseases.
As part of the treatment of coxarthrosis, patients are prescribed:
- drug therapy;
- exercise therapy;
- physiotherapy.
It is mandatory for all patients to take measures to eliminate the effects of factors that increase the load on the legs and contribute to the progression of degenerative changes in the hip joint. This includes adjusting your diet and increasing your level of physical activity if you are overweight. If the patient is regularly exposed to excessive physical exertion, it is recommended to change the type of activity or reduce the intensity of training, if the load is due to sports practice. In some cases, it is recommended to use special bandages and orthoses that fix the hip joint and unload it during physical exertion.
medical therapy
As part of drug treatment, patients are given individually selected drugs, taking into account existing concomitant diseases. As a rule, drugs from the following pharmacological groups are indicated for coxarthrosis:
- NSAIDs - an extensive group of drugs that exhibit analgesic and anti-inflammatory effects (available in various dosage forms, including tablets, capsules, gels, creams, injection solutions, allowing you to choose the most effective and convenient form of application);
- corticosteroids - drugs that have a powerful anti-inflammatory effect, but due to the high risk of side effects, especially when using oral forms, they are prescribed only for short courses in the form of injections;
- muscle relaxants - drugs that help reduce muscle tone, which allows you to effectively treat muscle spasms, which are often observed in coxarthrosis;
- chondroprotectors - a group of drugs that contain components used by the body for the regeneration of cartilage tissue;
- preparations that improve microcirculation - help to improve the nutrition of soft tissues and activate the course of metabolic processes in the affected area;
- B vitamins: are indicated for nerve conduction disorders caused by compression of the nerve by altered components of the hip joint.
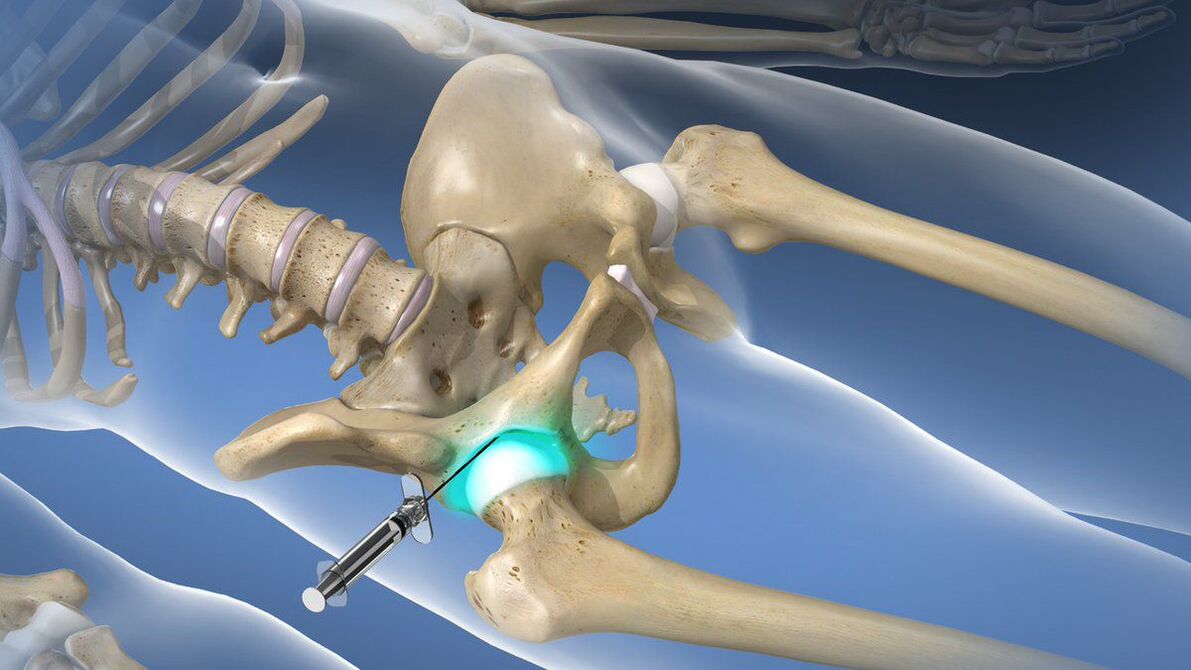
If the coxarthrosis caused an attack of acute pain, which cannot be stopped with the help of prescribed NSAIDs, then intraarticular or periarticular blockade is recommended for patients. Its essence lies in the introduction directly into the cavity of the hip joint of an anesthetic solution in combination with corticosteroids. This will allow you to quickly eliminate pain and reduce the inflammatory process. But the blockade can only be done by a qualified health worker in a specially prepared room. Performing such procedures at home is not shown.
exercise therapy
When diagnosing coxarthrosis, regular exercise therapy is mandatory. In the same way as drug therapy, a set of exercise therapy exercises is selected individually for each patient, taking into account the degree of destruction of the hip joint, the level of physical development of the patient, the nature of concomitant diseases (special attention is paid to cardiovascular pathologies).
Thanks to daily exercise therapy, you can:
- reduce the severity of pain;
- increase the mobility of the hip joint;
- reduce the risk of muscle atrophy;
- eliminate spasms of the thigh muscles;
- activate blood circulation and thus improve the nutrition of the affected joint.
All exercises should be performed gently, avoiding sudden movements and jerks. But if pain occurs during exercise therapy, you should definitely contact your doctor to correct the selected complex or make a new diagnosis to exclude the progression of the disease and the need for an operation.
Physiotherapy

Comprehensive treatment of coxarthrosis involves courses of physiotherapy procedures that have anti-inflammatory, analgesic, decongestant and tonic effects on the body. Therefore, most often patients are prescribed 10-15 procedures:
- ultrasound therapy;
- electrophoresis;
- UVT;
- magnet therapy;
- laser therapy etc.
Recently, plasmolifting has been increasingly used as part of the conservative treatment of coxarthrosis, which can significantly increase the rate of hyaline cartilage regeneration. The essence of the procedure is the introduction into the cavity of the hip joint of purified blood plasma, which is obtained by centrifugation of the patient's own blood.
Surgery for coxarthrosis
If a patient is diagnosed with coxarthrosis of the third degree, he is indicated for surgical intervention, since conservative methods in such cases no longer have power. Unfortunately, such situations are extremely common today, as a large number of patients seek medical help when they can no longer bear the pain or have serious mobility restrictions that deprive them of their ability to work and move independently.
Timely surgical intervention can completely eliminate these disorders and restore the patient's ability to move normally, significantly improving her quality of life. The indications for its implementation are:
- a significant decrease in joint space by more than 80%;
- the presence of severe pain in the hip joint, which cannot be eliminated;
- pronounced mobility disorders;
- femoral neck fracture.
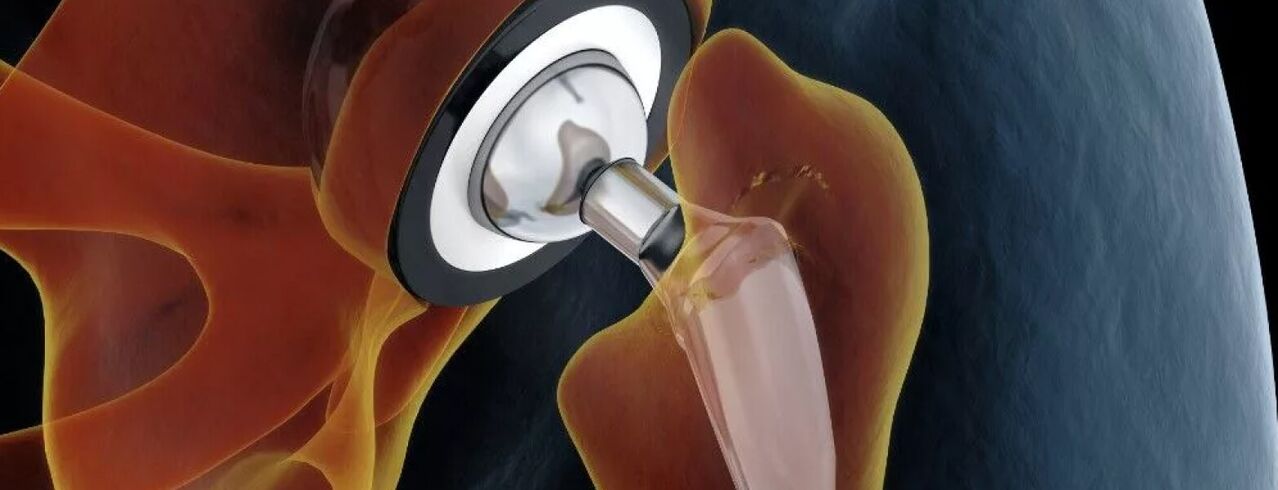
The gold standard for the treatment of severe coxarthrosis, even in the elderly, is hip arthroplasty. This operation involves the replacement of a destroyed hip joint with an artificial endoprosthesis made of durable and at the same time biologically compatible materials. Endoprosthesis allows you to fully restore the functionality of the hip joint, eliminate pain and return a person to a full-fledged active life.
The essence of this type of surgical intervention is the resection of the femoral head and a small fragment of its neck. In addition, the surgeon must prepare the surface of the acetabulum for the installation of the endoprosthesis, that is, remove all formed osteophytes and achieve maximum restoration of its normal shape. Subsequently, an endoprosthesis of the selected type is placed, which is fixed with a special cement (preferably for the treatment of the elderly) or uncemented. In the latter case, the endoprosthesis has a special spongy part in contact with the bone structures. Its fixation in the acetabulum is provided by the germination of bone tissue through the sponge.
For each patient, the type of arthroplasty is selected individually. The most effective is the total arthroplasty, which consists of the complete replacement of the entire hip joint, that is, the neck and head of the femur, as well as the acetabulum.
If the patient has preservation of normal hyaline cartilage on the surface of the acetabulum, she may undergo a partial arthroplasty with replacement of only the femoral head and/or neck. For this, endoprostheses of different designs are used: monopolar and bipolar.
The only disadvantage of arthroplasty can be considered the need to replace the installed endoprosthesis after 15-30 years.
After stent replacement, patients are shown rehabilitation, the duration of which depends on the rate of tissue repair. As part of recovery, exercise therapy, physiotherapy and therapeutic massage are prescribed.
Before the advent of modern endoprostheses, patients with grade 3 coxarthrosis were prescribed osteotomy or arthrodesis. Nowadays, these techniques are used less and less, since they have a number of disadvantages. Thus, arthrodesis involves the fixation of the bony structures of the hip joint with metal plates. As a result, the pain syndrome is completely eliminated, but the joint completely loses its mobility. Therefore, after arthrodesis, the patient can only stand, but can no longer walk independently due to lack of movement in the hip joint. Therefore, arthrodesis is practically not performed today.
Osteotomy involves the execution of an artificial fracture of the femur with a combination of bone fragments that will reduce the load on the affected hip joint. But the operation gives only a short-term effect, and in the future the need for arthroplasty still arises.
Therefore, coxarthrosis of the hip joint is quite a dangerous disease that can lead to disability. It seriously reduces the quality of life and deprives a person of the ability to work. But if you pay attention to the first signs of the pathology and consult an orthopedist in time, you can stop its progression and achieve a significant improvement in well-being. But with coxarthrosis already under way, there can only be one solution: arthroplasty. Fortunately, this method can be used even with severe degenerative dystrophic changes and fully restore the normal functioning of the hip joint.


























